Harnessing Phagocytic Immune Cells to Breach Cancer Fortifications
One of the most significant hurdles in combating metastatic cancer is the delivery of protein drugs to the affected sites. The cancer cells fortify themselves behind the body’s own structures—endothelial barriers and extracellular matrix—making it difficult for therapeutic agents to reach and destroy them. Employing phagocytic immune cells as Trojan horses to overcome these barriers has immense potential.
The Challenge: Endothelial and Matrix Barriers
The endothelial barrier, which lines the interior surface of blood vessels, serves as a selective filter, controlling the passage of substances, including drugs, into tissues. In cancer, the endothelium can be altered to become even more selective, preventing therapeutic agents from exiting the bloodstream and reaching tumor cells. Similarly, the extracellular matrix—a complex network of proteins and polysaccharides surrounding cells—can be dense and fibrous around tumors, creating a physical barrier that hampers drug delivery.
The Phagocytic Solution
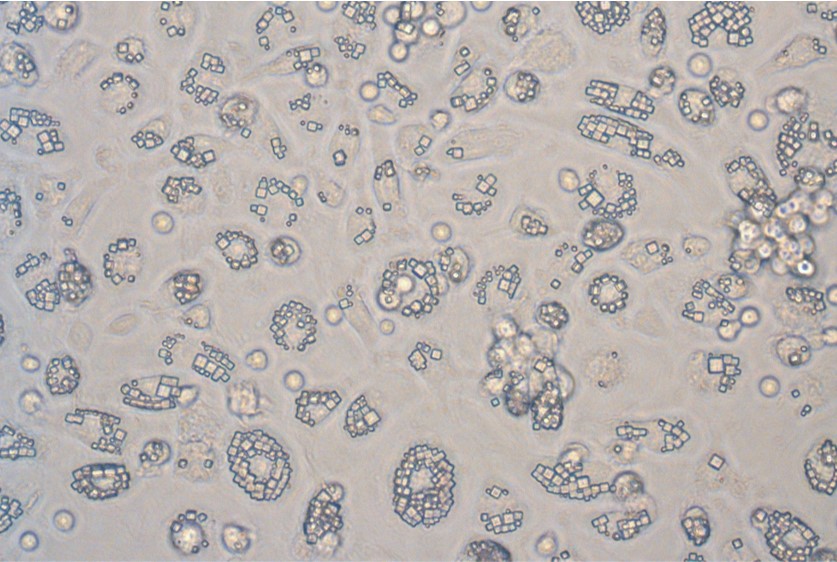
Phagocytic immune cells, such as macrophages and neutrophils, are the body’s natural defenders against pathogens. They have the unique ability to navigate through the body’s barriers and engulf foreign particles. At Cell Guidance Systems, we are exploring ways to harness these cells’ natural trafficking abilities to deliver protein drugs directly into the sites of metastatic cancer.
The concept is elegant in its simplicity: by encapsulating protein drugs within phagocytic cells, we are using these cells as vehicles to transport the drugs through the endothelial and matrix barriers. Once at the tumor site, the phagocytic cells can release the therapeutic agents, allowing them to exert their effects directly on the cancer cells or bosting the anti-cancer activity of other immune cells. The strategy helps to reduce degradation and kidney filtering of the drug in the serum. This reduces drug dosing and potential for off target toxicity.
The Trojan Horse Strategy
This approach is akin to the ancient tale of the Trojan Horse. The phagocytic cells, loaded with protein drugs, would be the ‘horse’ allowed to pass through the ‘gates’ of the endothelial and matrix barriers, unsuspected by the ‘defenders’—the cancer cells. Upon reaching their target, these cellular vehicles would then deploy their ‘warriors’—the protein drugs—to attack the cancer cells from within their own stronghold.
The Promise and the Hurdles
The potential benefits of using phagocytic immune cells for drug delivery are immense. This method could increase the concentration of drugs at the tumor site, reduce systemic side effects, and improve the overall efficacy of cancer treatments. We are refining the approach to address targeting efficiency: Ensuring that the phagocytic cells loaded with drugs are efficiently homing to the tumor sites without getting sidetracked or trapped in other tissues.
The Road Ahead
The use of phagocytic immune cells to overcome endothelial and matrix barriers represents a frontier in cancer therapy. While preclinical studies have shown promise, translating these findings into clinical practice will require rigorous testing and refinement. The road ahead involves detailed understanding of tumor biology, the microenvironment, and the intricate behaviour of immune cells within the body.
As we continue to unravel the complexities of this approach, there is hope that we can usher in a new era of precision medicine where the body’s own cells are empowered to become targeted drug carriers. This could lead to more effective treatments for metastatic cancer, as well as other diseases, offering hope to patients who currently have limited options.
IMAGE: MAcrophages engulfing PODS protein crystals, Cell Guidance Systems
Learn more about powerful technologies that are enabling research: